Beta blockers take on new life in heart disease
Beta blockers have been shown to regulate heart function when it is most needed in a growing group of patients at risk of cardiac arrest.
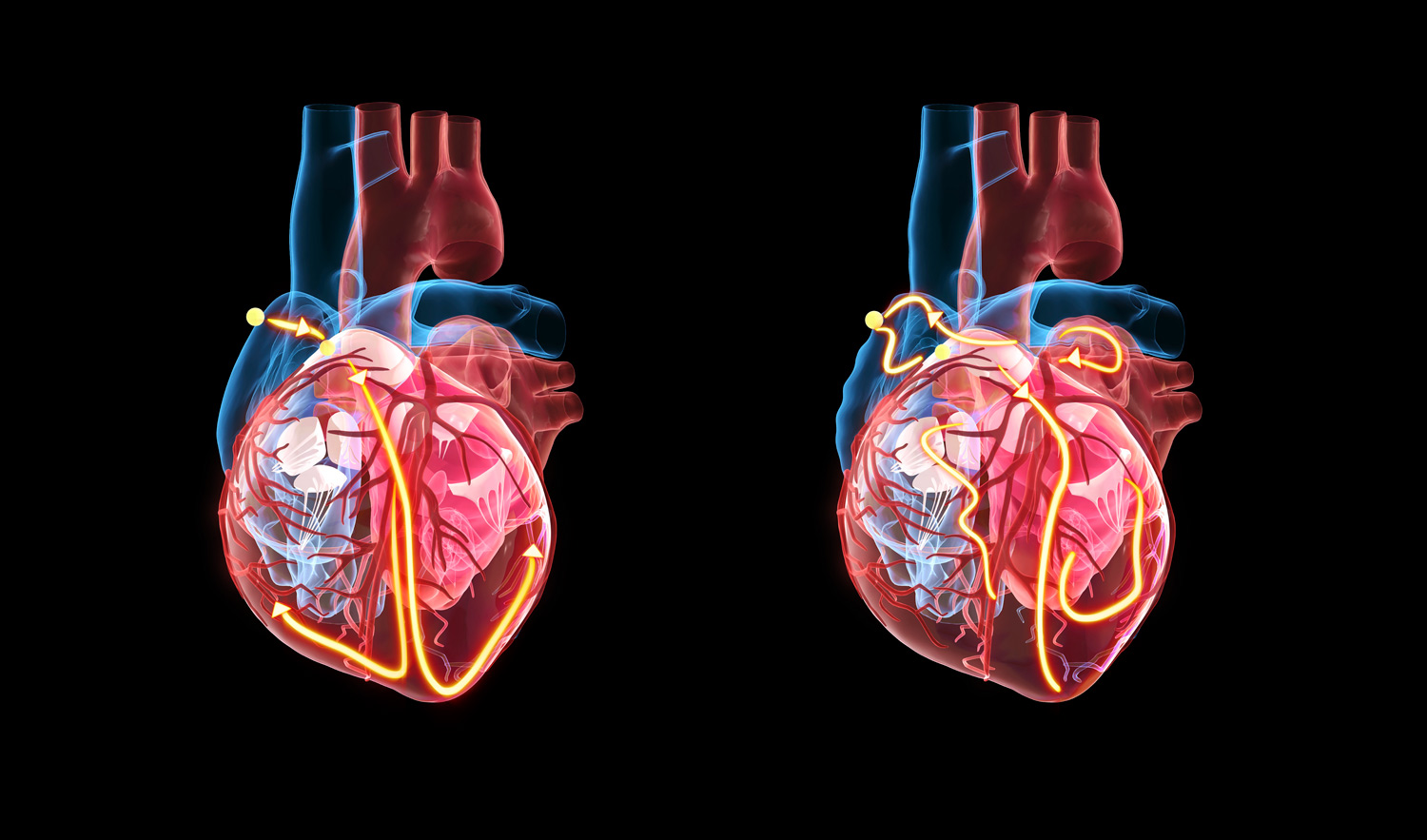
Heart failure is a lifelong condition in which the heart muscle can’t pump enough blood to meet the body’s needs. Different types of heart failure are categorised based on the ejection fraction, which indicates the percentage of blood pumped out of the heart with each heartbeat. One form, known as heart failure with preserved ejection fraction (HFpEF), involves a maintained ejection fraction with no significant decline and is becoming increasingly common. It is often associated with sudden death due to abnormal heartbeats called ventricular arrhythmias.
A study by researchers at Khalifa University suggests that beta-blocker drugs could protect patients with this form of heart disease, reducing the risk of cardiac arrest and death.
We detected improved control of heart-rate variability with beta blockers, especially at times associated with high cardiac risk
Heartbeat is controlled by an interplay between the sympathetic and parasympathetic nervous systems. The sympathetic system accelerates heart rate in response to stressful situations; while the parasympathetic system acts to maintain a steady and slower heart rate.
Beta blockers inhibit overstimulation of the sympathetic nervous system. While they are widely used in patients with reduced ejection fraction, their effects on patients experiencing HFpEF have been unclear until now.
Researchers at Khalifa University studied beta-blocker administration in patients with HFpEF by monitoring the effects on heart activity at different times of the day using electrocardiogram (ECG) testing.
“We detected improved control of heart-rate variability with beta blockers, especially at times associated with high cardiac risk,” says biomedical engineer Leontios Hadjileontiadis of the Khalifa team. “This suggests that beta-blocker therapy might significantly protect patients with HFpEF.”
Hadjileontiadis emphasises that HFpEF is a variable condition that requires treatment tailored to the specific needs of each patient. Insights gained from this study could help to personalise treatment. By monitoring the patients regularly over 24 hours, the study identified a particularly significant improvement and overall decreased risk of a dangerous cardiac event in the early morning. At that time of day, the risk is increased due to a surge in activity by the sympathetic nervous system.
“Prescription of beta blockers could target high-risk time periods to effectively regulate the heart’s function when it’s most needed,” says Hadjileontiadis.
The initial results were from a small, short-term study of 56 treated patients and 17 controls. The team is planning to carry out longer-term treatment and monitoring, and will explore different beta blockers, as well as the effects of variables such as patients’ sex, age, ethnicity and other medical conditions. The researchers are also developing artificial intelligence approaches with the potential to refine the interpretation of heart-function data and guide the choice of treatment options.
Reference
1. Saleem, S. et al. Investigating the effects of beta-blockers on circadian heart rhythm using heart rate variability in ischemic heart disease with preserved ejection fraction. Scientific Reports 13, 5828 (2023). | Article